Provisional diagnosis: ALCOHOLIC GASTRITIS ACUTE PHARYNGITIS (? REACTIVE ? INFECTIVE ) WITH AKI RESOLVED DENOVO DM ( HBA1C 6.9)

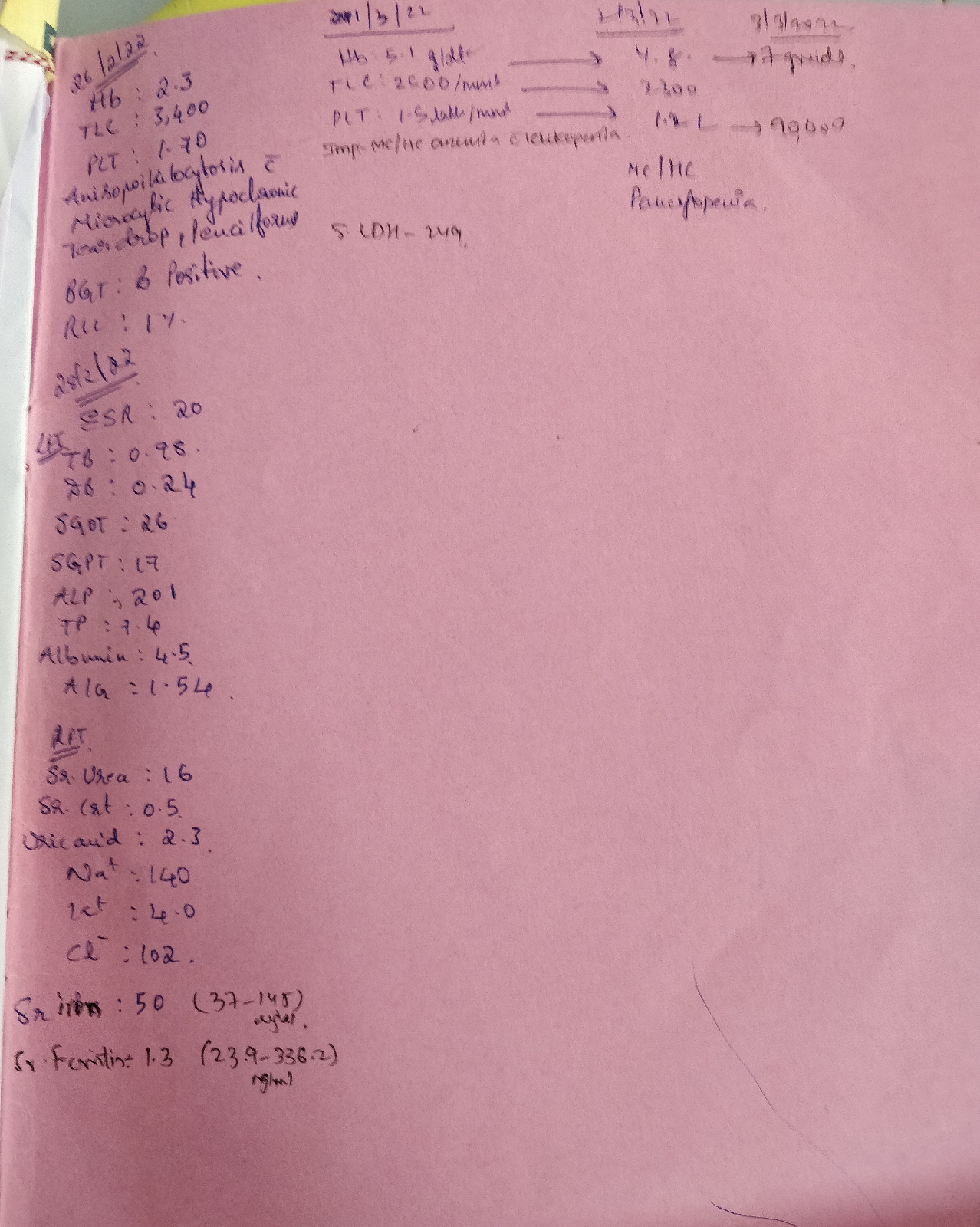
Patient came to casuality wih c/o epigastric pain since 2pm of 27/2/22. Nausea and vomitings are present since 4pm yesterday. HOPI: Patient is a chronic alcoholic since 20yrs. Due to issues with his wife, he is consuming alcohol since 1yr. For the last 7days he is drinking wihout having food. C/o epigastric pain since yesterday Burning type, radiating to back gradually progressive. Nausea present, vomitings present of dark black colored. Non bilious, non projectile. C/o Burning sensation in throat Similar episode of binge drinking 2 eisodes in last 1yr. K/C/O HTN since 5yrs , on medication - irregular. N/K/C/O: DM, TB, asthma. O/E: Pt is C/C/C. Afebrile. Bp: 120/80 Pr: 84 bpm Rs: BAE+ CVS: S1S2 + CNS: NAD. Abdomen : soft and tender at left hypochondrium After TREATMENT :- 1) INJ PANTOP 40 MG OD 2) INJ THIAMINE 100 MG IV BF 3) IVF NS AND RL 4) INJ ZOFER 4 MG...